Treatment for Prostate Cancer
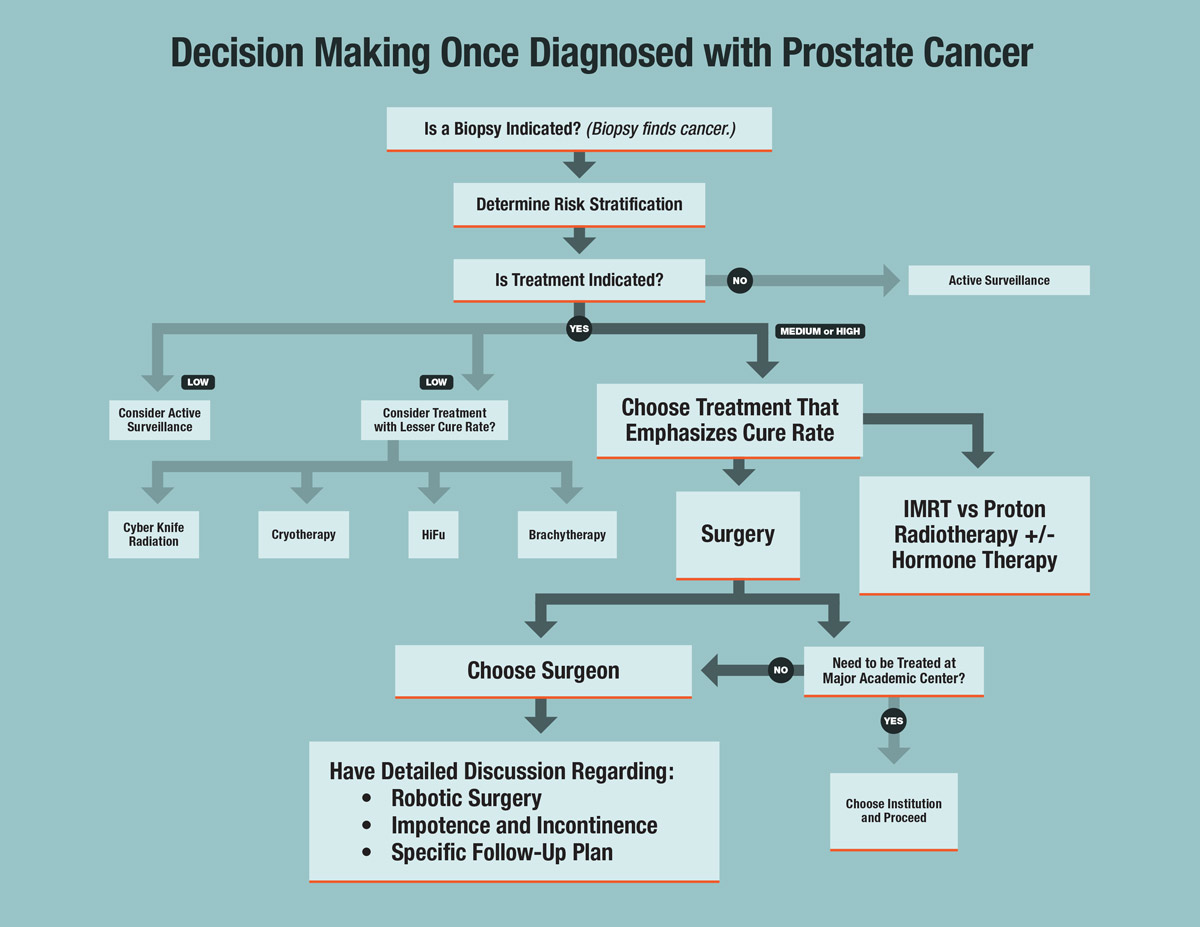
For patients where there is enough evidence to suggest that one’s prostate cancer will progress at a pace that would potentially shorten life span, treatment of some sort is indicated. Deciding to undergo active surveillance or not is certainly a challenge, but deciding on treatment is often the hardest part of the process for some patients. There are options; in some cases, there are too many for the patient to sort out easily.
Risk Stratification’s Role in Determining the Path Forward
No Risk & Low-Risk Prostate Cancer: Consider Active Surveillance
In our previous essay found in the prostate cancer section of the Common Problems tab on our website, we discussed the importance of understanding cancer, prostate cancer, one’s pathology report, and, most importantly, risk stratification to determine a proper course of action. In Dr. Engel’s vernacular, no-risk and low-risk patients usually are within the Gleason score six groups and are either older patients or patients where no suspicious PSA rise has been seen and/or little cancer was found on the biopsy. We urologists call this “insignificant” cancer, and it took many years of overtreatment to understand that such cancers are usually best off not being treated, at least at first. The concept of not treating prostate cancer was first called Watchful Waiting, meaning no treatment would ever be offered. We now call this Active Surveillance. It is important to understand that active surveillance is a recognition that the parameters do not provide enough convincing evidence that one’s prostate cancer is significant, so more data is needed before opting for treatment. In Dr. Engel’s hands, that data comes in the form of regular PSA testing and rectal exams, and at least one more biopsy is usually done one year from the first biopsy in a far more sensitive way called a saturation biopsy. MRI is also used as part of active surveillance to look for changes that could be targeted during that biopsy with a technology called MRI fusion. Some genetic tests are designed to predict the likelihood of disease progression or whether active surveillance is the best approach. Examples are Prolaris, Oncotype DX, and Decipher, amongst others. These tests usually have little utility for Dr. Engel’s practice as he is already far more discriminatory than most in offering a prostate biopsy in the first place. If a Urologist insists on several successive PSA rises or a higher threshold number, one can already relatively safely assume cancer growth if the PSA does not level out during active surveillance, and these tests then offer little prognostic information in this setting. It is for these reasons, as well as unnecessary costs, that Dr. Engel rarely uses them. Most patients who start active surveillance with Dr. Engel are never treated, but patients are closely monitored to look for exceptions.
Cases When Treatment Is Indicated
For patients where there is enough evidence to know that one’s prostate cancer will likely progress and shorten one’s life span, as with younger patients, patients with just a little too much cancer found to be comfortable, a suspicious PSA trend or Gleason score perhaps higher than six, treatment of some sort is usually indicated. This is where the hard part can start for some patients. There are options; in some cases, there are too many options for the patient to sort out. There is marketing, and it is often hard for a patient to discern between education and marketing. There are very few head-to-head studies to choose a clear winner and thus, often no “right answer.” Every patient learns differently, and some things resonate more than others. Dr. Engel calls the process of becoming comfortable with a particular course of action the “journey” of prostate cancer. What is done at USW is to encourage this process and hopefully allow the patient, with some counseling, to develop a gut leaning towards or away from different treatments. As you will see below, the treatment offerings for prostate cancer could not be more diametrically opposed in their approach. If one realizes this and ensures they are choosing a treatment appropriate for their risk stratification, this gut learning, and not pure science, is the best guide. We feel that our job as a tour guide for this journey is to make sure that this learning is not based on misunderstandings or false expectations that often occur when based solely on internet-based learning.
If there is an appreciable risk of metastasis or spread based on the risk stratification, her first step will be to get some combination of tests to look for spread. These tests include a CT scan, a standard bone scan, or, more recently, a Prostatic Surface Membrane Antigen (PSMA) scan. PSMA scans have become a mainstay test for oncologists and radiation oncologists and are obtained when a higher level of sensitivity or specificity are needed. An insurance company does not always approve them.
Below are some general ideas and concepts. Here, we have tried to make each treatment option available to be further reviewed by clicking on that option, so please do so to learn more. There are separate pages for many treatments listed below where you can learn even more, see operative videos, and focus on the actual pre-procedure and post-procedure details.
In general, one will not find a unanimous consensus, even within each risk stratification, but there are some general rules. All patients are looking for the option with the highest cure rate and fewest side effects, and there are some circumstances where there can seem to be a clear winner, at least to Dr. Engel. Realize that what you see here, therefore, broadly represents his opinions and not fact. Also, there is no substitute for consulting with an expert like Dr. Engel or another experienced urologist or radiation oncologist to determine one’s individual risk stratification and what treatment is right for you.
Lower Risk & Moderate Risk Prostate Cancer
If Active Surveillance is ruled out as an appropriate option, patients in this category have the most options and often the hardest decision to make. A patient will have to decide first if they may be interested in the various forms of treatment that generally have perceived lesser cure rates. At first glance, choosing a treatment with a lesser cure rate may make no sense, but when put in the context of one’s case, it certainly can make sense. For instance, such treatments might fit very well if a patient’s risk stratification is just above the threshold for active surveillance but still low risk, an older patient or a patient with multiple medical problems, etc. This grouping of treatments includes two forms of radiation called CyberKnife and brachytherapy/seeds (rarely performed anymore), and also cryotherapy (freezing the prostate) and high-intensity focused ultrasound/HIFU (heating the prostate). There are also centers performing ablation to only localized areas of the prostate, but we know now that patients who qualify for this treatment these days are usually better served by active surveillance. All of these treatments have distinct pros and cons, to be discussed further below, but all are performed in an effort to reduce side effects or lessen the general burden of treatment when treatment is indicated.
Most patients, when understanding the cure rate tradeoff of these treatments, still choose treatments that do prioritize cure, and this leads them to choose either surgery or external beam radiation. For a long time, within this risk group, Dr. Engel largely encouraged patients to lean on their gut feeling more than anything else to decide what treatment to choose here. There is an acuity to surgery and a closure with surgery that does not come with radiation, but for some, this acuity is too daunting to accept. Both surgery and radiation have side effects, but different ones. The concept of “pick your poison” is often applied here with the idea that both treatments have downsides, just of different flavors. These days, however, radiation protocols usually involve at least six months of hormone therapy included as part of a lower-risk radiation protocol to improve the cure rate. This treatment drops a man’s testosterone to zero and adds another set of side effects, and thus more poison, to the radiation choice. It will also mask the PSA and thus prevent a patient from knowing if treatment was effective for a long time. There is also the fact that sometimes, testicular function is very slow to return. Now that hormone therapy is usually used, one might argue that surgery has fewer overall side effects. But this is for the patient to decide.
In most series, including Dr. Engel’s experience, younger people tend to strongly favor surgery, whereas patients closer to 70 or beyond may find the concept of radiation, including its daily treatments for several weeks and concomitant hormone therapy, easier to accept and in ways more appealing. But again, there are no hard and fast rules here in this low/moderate risk stratification group.
High-Risk Prostate Cancer
For high-risk patients, Dr. Engel feels strongly that surgery is the treatment that most approximates the ideal of the highest cure rate and fewest side effects.
For high-risk patients, Dr. Engel feels strongly that surgery is the treatment that most approximates the ideal of the highest cure rate and fewest side effects. A high-dose radiation regimen is certainly an alternative. This consists of a lengthy course of external beam radiation (either standard IMRT or proton is almost equivalent) plus at least two years of hormone therapy and possibly a second radiation modality such as CyberKnife or brachytherapy (seed implantation). Even with this highly aggressive radiation approach, few studies have shown radiation to offer the cure rate that surgery does, and no head-to-head studies exist. Hormone therapy masks whether a patient is cured or not, and arguably, the combination regimen of high-risk radiation protocols has far more overall impact on one’s life than surgery alone would have. Also, the patient is left not knowing if the treatment worked for almost three years, and many find this limbo state unacceptable. Surgery will produce a pathology report that will guide whether added radiation after surgery makes sense or not, and the lack of hormone therapy after surgery will tell a patient their cure status right away. It will allow for a fuller understanding of the proper next steps in treatment. Dr. Engel has published an often-quoted study on the success of robotic surgery alone in high-risk settings (see Bibliography in his profile), and this research cemented his strong leaning toward surgery for these patients. Patients in this group are highly encouraged to seek a radiation opinion to learn more, and some will undoubtedly choose radiation to treat their case. Once fully educated on all of these pros and cons, most in Dr. Engel’s practice usually choose robotic prostatectomy in these high-risk situations.
Treatments For Prostate Cancer
Below, we will touch upon the most popular treatments for prostate cancer currently available. We have included the most common and some rarely used treatments to be complete. In many cases, several treatments listed below can be found under their separate tab under the Common Treatments section. Please learn more there as we use these pages to educate our patients regarding the specifics of procedures, show operative videos, and answer frequently asked questions.
Less Aggressive Prostate Cancer Treatments That Do Not Prioritize Cure
Cryotherapy for Prostate Cancer
Dr. Engel offers cryotherapy for prostate cancer and, in some cases, feels it is the perfect fit. Such patients might include an older patient with highly significant prostate cancer and thus not a good candidate for active surveillance, an older patient not a good candidate for radiation due to urinary difficulties, or one whose pathology report and parameters don’t seem to warrant highly aggressive management.
Cryotherapy was initially developed as a way to treat patients who recurred after radiation since surgery is not a wise option in such patients. It used the same technology as brachytherapy, except here needles that delivered very cold gasses are placed to kill prostate tissue. It is done in real-time and visualized and controlled with ultrasound and temperature sensors. It offers a cure rate similar to radiation but probably not as good as surgery. But, unlike radiation, cryotherapy can be repeated years later if cancer does recur. Cryotherapy will have the same or worse effect on erections as surgery but does not have the mandatory period of incontinence that surgery brings. Cryotherapy has the same low risk of incontinence and rectal fistula formation as radiation. Dr. Engel makes sure all of his patients review this option, as well as surgery and radiation, when learning about prostate cancer and its treatments.
High-Intensity Focus Ultrasound (HIFU)
This treatment was popularized in Europe and was introduced in clinical trials ten years ago but did not get FDA approval due to a high complication rate. Some U.S. providers still offered this as a minimally invasive treatment overseas for cash during this time, but now there is FDA approval. This treatment is very similar to cryotherapy in that it also destroys prostate tissue, only here ultrasonic waves are used to generate heat and not cold. Dr. Engel feels that HIFU is in many ways interchangeable with cryotherapy, but HIFU seems to have more complications and a far higher rate of not being able to urinate after the procedure. HIFU was initially introduced as a means to ablate only a small area of the prostate selectively. Cryotherapy was also used in this way. These were always low-risk patients; we now know these patients are usually best served only with active surveillance.
Many HIFU patients will need a second procedure called a TURP to allow them to urinate. This is rarely seen with cryotherapy, and most patients actually urinate far better long-term after cryotherapy. For these reasons, Dr. Engel has not adopted HIFU into his practice, and in those cases where cryotherapy or HIFU would be applicable, he prefers to recommend cryotherapy.
Radiation Therapy for Prostate Cancer
Radiation therapy can be a good choice as long as one understands the side effects of radiation, both short-term and long-term, and the lack of closure that sometimes occurs with it. The field of radiation oncology is dynamic, and technology continuously improves the ability to deliver radiation in a more focused beam. This allows for a higher dose, and hopefully, with that comes higher cure rates. Radiation Oncology is extremely research-driven, and as new technology progresses or new theories on cure rate improvement are fomented, large multi-center research trials are then performed to evaluate new protocols. Thus, the protocols used today may change later. A good example of this is how such trials went from recommending six months of hormone therapy to high-risk cases to now recommending this in lower-risk cases and two to three years of hormone therapy in high-risk cases.
The goal here has always been to give radiation in a more focused way to allow for higher doses with less effect on neighboring organs like the bladder and rectum. Thus, over the years, we have seen open placement of radioactive seeds go to needle placement of radioactive seeds (brachytherapy), then to better external beam machines and ways to deliver external beam (3D conformal and IMRT), now to Proton Beam. CyberKnife is the most focused, and some would say too focused to allow for overlap beyond the edges of the prostate.
It can be very hard for patients to understand this progression of technology, and marketing does not help. Proton beam is highly marketed now, for instance, but most experts agree it does not offer a significant advantage over contemporary standard external beam radiotherapy, at least for now. Below, we will try to give a summary of these modalities. Of course, we will help arrange a consultation with a radiation oncologist for a more detailed discussion.
Cyberknife Radiation
CyberKnife radiation is a particularly appealing choice at first glance because it is the most focused, with a whole course consisting of only five treatments. However, Dr. Engel reserves recommending this only to older patients, those with co-morbidities, and those with low-risk cancer due to its lack of long-term cure rate data to show equality with longer external beam radiation protocols that are specifically designed to maximize cure (3D conformal, IMRT or Proton). CyberKnife probably does cause fewer side effects, particularly with regard to erectile function. However, there is every reason to assume that cure rates in higher-risk stratification groups also are lower. By giving such high doses each day to allow for a five-day total course, the rectum and bladder must not be treated as they could not withstand this radiation. This disallows treatment to the edges of the prostate at times and certainly does not allow for a margin of treatment around the prostate. Patients must understand this tradeoff when choosing this modality. Also, some radiation oncologists are starting to use hormone therapy for usually six months in conjunction with CyberKnife Radiation for all but the lowest risk stratifications. Dr. Engel supports CyberKnife for lower-risk cases and often recommends it, but for now, he does not recommend this modality for anything higher than low-risk or low/moderate-risk older patients.
Brachytherapy for Prostate Cancer
Brachytherapy, or prostate “seeding,” is declining in popularity but is still performed at a few sites in the DMV. Seeds were the original minimally invasive therapy, and in the late 90s, as many people had seeds as they underwent surgery (open surgery at that time). There were many head-to-head comparisons back then comparing seeds to surgery, and it ultimately showed that seeds were not effective for Gleason scores higher than six and that the overall side effect profile was worse than surgery. For Dr. Engel, CyberKnife has largely replaced brachytherapy in his practice for those patients with lower-risk cancer willing to accept a lower cure rate and unwilling to undergo surgery.
External Beam Radiation for Prostate Cancer
As stated above, the technology used to fire radiation particles from outside the body through parts of the body has continuously progressed and likely will continue to progress. Until recently, this progression had to do with the evolution of more advanced machines capable of generating radiation particles and delivering them in a more precise, localized way. Different technologies accomplish this differently, and we see small improvements in new technologies. Examples of breakthroughs include Intensity Modulated Radiation Therapy and 3D Conformal Radiation Therapy. These were revolutionary improvements in delivering standard X-ray particles called photons. Now, new machines generate different particles called protons. Hopefully, with this new platform, we will see the same small steps forward that will eventually allow proton therapy to be the clear winner. However, as of right now, these modalities are all close. Many patients refer to proton therapy as very different, but Dr. Engel considers all of these contemporary modalities similar when delivered by a skilled radiation oncologist.
These modalities will have early side effects involving fatigue later in the course due to cellular damage and effects stemming from irritation to the bladder and rectum, such as frequent urination and defecation. These usually resolve within three months or so. These modalities also often exhibit mid-term effects, perhaps a few years later, that have to do with scarring. This is when patients might develop incontinence in approximately 4% or so, urethral strictures, and other tissue-related problems. Late side effects include bladder hemorrhage called radiation cystitis, and secondary malignancy risks.
You will learn below that external beam radiation is very different than surgery. It has side effects, but different side effects. It is a relatively long course, sometimes up to eight or nine weeks, and will involve a variable period of hormone therapy dictated by one’s risk stratification. Knowing its efficacy by seeing the PSA go down to very low levels will be delayed by one year if no hormone therapy is used and far longer if hormone therapy is used. However, it does not have the acuity of surgery that sometimes just does not fit one’s personality type and is perfect if surgery represents a significant risk. We often suggest that radiation matches patients who are luckily able to worry about what comes tomorrow later – patients who live day by day and thus will not need to know that they are cured to stave off anxiety and simply do not want to face all their possible side effects head on as must be done with surgery.
Surgical Treatment for Prostate Cancer
The mainstay of prostate cancer treatment, and the one most often performed by Dr. Engel, is surgery. Dr. Engel had performed hundreds of open surgeries in the form of nerve-sparing radical retropubic prostatectomy (RRP), but in 2004, he helped introduce robotic prostatectomy in the mid-Atlantic area and now exclusively performs robotic prostatectomy and is proud to see have become the dominant approach to prostate surgery today. He has performed over 3000 such surgeries. He is considered a pioneer in robotic surgery and associated outcomes research. He was the first to perform such cases in the mid-Atlantic region through his development of the robotic surgery program at George Washington. Please go to our dedicated Robotic Prostatectomy page in the Common Procedures section of our site for a detailed discussion.
Robotic Prostatectomy stands as the gold standard of cure by which all other treatments are measured. High-dose external radiation protocols also enlisting hormone therapy are considered to offer very similar cure rates. In many ways, radiation and surgery could not be more different treatments. With surgery, there is the acuity of having an actual surgery date, and that can either be welcomed as the day that one will have their problem fully dealt with and a hopeful cure achieved, or that can be very anxiety-producing for some. The surgery’s main two side effects occur immediately after surgery. First, the bladder must heal after surgery, which means that all patients will go through a period of leaking at least some of their urine after surgery. Patients will have to wear pads, and the number and for how long can vary. Typically, patients are out of pads at their three-month PSA visit. Some get dry far sooner, and some later. There is the same number of patients who will have some degree of permanent incontinence as with radiation – 4-5%.
All robotic prostatectomy patients will also lose their erections after surgery. If they return, and how fast they return, very much depends on how good one’s erections are before surgery, comorbidities, one’s relationship with their sexual partner, and one’s cardiovascular health. This can be daunting to a patient, but unfortunately, radiation, where the trouble with erections happens in a delayed fashion when no hormone therapy is used, will also take away erections right away while hormone therapy is being utilized. This fact causes some to look hard at treatments that do not prioritize cure, but again, this will be at the cost of a lower cure rate.
The good news with surgery, though, is that patients typically stay only one night in the hospital and feel fully recovered other than having to regain their incontinence in two weeks. Erectile dysfunction can be aggressively managed while we are waiting for one’s erections to recur, and incontinence is almost always temporary and not life-altering. Surgical risks such as injury or bleeding are very low in experienced hands, and patients will know they are cured by seeing an undetectable PSA result. For many, this closure that surgery provides is priceless.
Again, please review the tabs under the Common Procedures tab on this site for more information on individual procedures such as Robotic Prostatectomy and many others.